Abstract
In order to investigate safety and immunogenicity of SARS-CoV-2 vaccine third dose in people living with HIV (PLWH), we analyze anti-RBD, microneutralization assay and IFN-γ production in 216 PLWH on ART with advanced disease (CD4 count <200 cell/mm3 and/or previous AIDS) receiving the third dose of a mRNA vaccine (BNT162b2 or mRNA-1273) after a median of 142 days from the second dose. Median age is 54 years, median CD4 nadir 45 cell/mm3 (20–122), 93% HIV-RNA < 50 c/mL. In 68% of PLWH at least one side-effect, generally mild, is recorded. Humoral response after the third dose was strong and higher than that achieved with the second dose (>2 log2 difference), especially when a heterologous combination with mRNA-1273 as third shot is used. In contrast, cell-mediated immunity remain stable. Our data support usefulness of third dose in PLWH currently receiving suppressive ART who presented with severe immune dysregulation.
Similar content being viewed by others
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) pandemic has led to more than 270 million confirmed cases of COVID-19 and about 5 million deaths1, as reported by the World Health organization up to December, 27th 2021. Effective vaccines licensed against SARS-CoV-2, with more than 7 million doses administered worldwide1 have proved to be a highly successful strategy to reduce the disease burden, particularly in people at high risk of developing a severe COVID-192. In addition, real-world data suggest that an effective vaccination is successful in preventing severe disease and death even in the presence of variants of concern (VoCs)3,4 such as Gamma and Delta variants, and many countries regulatory authorities indicate a third additional dose (AD) as necessary to maintain an adequate protection to SARS-CoV-2 and to the VoCs, especially for susceptible sub-populations5,6.
More recently, serious concerns are arising for the emergence of the B.1.1.529 (Omicron) variant because it has been shown that vaccine effectiveness is significantly lower than that seen with the delta variant, limiting the antibody-mediated neutralization and possibly increase the risk of reinfections7,8,9,10 Several studies recently supported a significant increase of neutralization against Omicron after a booster dose, although this increase was lower than that observed with ancestral type or Delta7,8,9,10,11, suggesting a cross-reactivity of neutralizing antibody responses10,11.
Although with discrepancies between studies, people living with HIV (PLWH) appear to be a high-risk group for adverse clinical outcomes from COVID-19, with some evidence for higher hospitalization and mortality rates12,13,14 that might be due to a poor neutralizing antibody titres reflecting a reduced antibody response to SARS-CoV-2 natural infection15 as well as to the presence of additional comorbidities and low socioeconomic status or occupational risk16.These data are consistent with the observation that HIV infection may favor a poor serological response to other viral agents, such as influenza17.
Up to date, only one randomized, phase 2/3 trial in UK have described both immunogenicity to a prime-boost dosing of the chimpanzee adenovirus-vectored ChAdOx1-nCoV-19 vaccine in PLWH on stable ART and with CD4 counts > 350 cells/mm3,18 and its durability after 6 months19. This follow-up analysis showed a decline in humoral and cell-mediated immunity, at 6 months, although with no significant difference compared to a cohort of HIV uninfected individuals vaccinated with the same vaccine.
Regarding mRNA vaccines in PLWH, to date only few observational studies exist and all showed a satisfactory humoral20,21,22,23,24,25,26 and T cell immune response20 in PLWH on ART and with CD4 T cell counts above 200 cell/mm3 after primary vaccination cycle, but no information was available about efficacy and safety of additional or booster dose in HIV-infected population, especially in people with low CD4 count.
We previously reported that mRNA vaccination is able to elicit a robust humoral and cellular immune response against SARS-CoV-2 in most of PLWH receiving ART, particularly in those with full immune recovery after suppressive therapy, even though such response was significantly poorer in PLWH with current CD4 T-cell < 200/mm3 compared to those with > 500 cell/mm3 and HIV-uninfected controls. These results suggest that chronic persistent dysregulation in ART-treated population may affect the effector immune response to SARS CoV2 vaccination27.
On September 10th, 2021, the administration of a third dose of anti-SARS-CoV-2 mRNA vaccine was approved in Italy to be given after >28 days after completion of the primary vaccination cycle in PLWH (to be intended as a full additional dose vaccine) who presented with a CD4 T cell count <200/mm3 and/or previous AIDS at the time of their first dose. The aims of this analysis were to investigate reactogenicity and degree of immunogenicity after the third dose in PLWH, to compare the levels to those achieved after the second dose and to evaluate the association between immune response and current CD4 T cells count and specific vaccine sequence.
Results
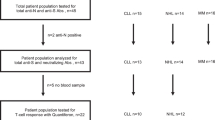
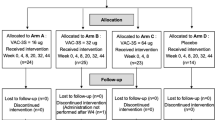
A total of 216 PLWH were included in the analysis (PCDR = 44; ICDR = 96; HCDR = 76). The main characteristics of HIV-infected participants according to current CD4 T cell count strata at time of third dose are reported in Table 1. Briefly, the median age was 54 years old (IQR 47, 59); all HIV patients were on ART at time of third dose, 92.6% had HIV-RNA < 50 copies/mL with a median time since HIV diagnosis of 7 years (3–12) and of 5 years (2–8) since AIDS, if diagnosed; 6.9% with a diagnosis of cancer; the three groups significantly differed for CD4 count nadir (p = 0.007), previous AIDS diagnosis (p < 0.001), time since AIDS diagnosis (p = 0.001), HIV-RNA (p < 0.001) at third dose. Proportion of PLWH with HIV-RNA lower than 50 copies/mL at the time of third dose was 79.5% in PCDR, 93.8% in ICDR, and 98.7% in HCDR (p < 0.001). More details on CD4 transition in CD4 count from baseline (the time of first dose) to T0 (time of third dose) are shown in supplementary table 1. The median time from the date of primary vaccination series to third dose was 142 days (132–156), longer for PCDR than ICDR and HCDR [154 (134,159) versus 145 (132,157) and 138 (130–151); p = 0.006].
The HCWs group was mainly composed by female subjects [72/98 (73.5%) vs 39/216 PLWH (18%); p < 0.0001], with a younger median age 44 years old (IQR 32–52) than PLWH (54 years old (47–59), the median time between the third dose and response measurement was 16 days (14–18), shorter than that observed in PLWH [33 days (30–35)], as well as, the interval of response measurement between T−1 and T0 was was significantly longer than PLWH [285 days (280, 291) vs. 117 (103,126)].
We identified n = 44/214 (20%) participants who received BNT162b2 vaccination for all the 3 doses and n = 80/214 (37%) to mRNA-1273 for all the three doses, n = 57/214 (26.6%) received as primary series BNT162b2 and for third dose mRNA-1273, whereas, n = 31/214 (14.4%) received mRNA-1273 as primary vaccination and BNT162b2 as third dose. There were two participants with a sequence involving not mRNA vaccines (one ChAdOx-ncov-19 followed by mRNA-1273 and one Ad26.COV2.S followed by mRNA-1273) which have been excluded from the regression analysis.
In a subset of the study population for whom a value of the response was available at time T−1, we compared the level of immunogenic response post third dose with that achieved 1 month after the 2nd dose of vaccination. The humoral response elicited by third dose was on average stronger than the titres elicited by the primary vaccination 1 month after the completion of 2 doses vaccination cycle (time T−1) although different timepoints post-vaccination are compared.
The comparison of the mean log2 of anti-RBD IgG between T−1 and T1 was performed in N = 169/216 patients and these means were: 9.8 BAU/mL (SD 2.9) at T−1 and 11.8 (SD 2.1) at T1 (p = 0.003) with an estimated mean log2 increase of 2.0 (SD 1.6) (p < 0.0001) (Fig. 1A).
A–C Mean log2 change of anti-RBD IgG (A),MNA90 (B) and IFN-γ (C) from 1 month response after the 2nd dose (T−1) and after the 3rd dose (T1) [Paired t-test, 2-sided no adjustment for multiple comparisons]. Mean Log2 changes of anti-RBD IgG (A) and MNA90 (B) significantly increased from T-1 to T1 (p < 0.0001; p < 0.0001; respectively but IFN-γ (C, p = 0.39) Source data are provided as a Source Data file.
The mean log2 of nAbs (available for N = 75/216 patients) were: 4.9 (SD 2.2) at T−1 and 8.3 (SD 2.4) at T1 (p = 0.018) with a mean increase of 3.4 (SD 2.1) (p < 0.0001) (Fig. 1B).
The mean log2 of IFN-γ (available for N = 74/216) were 6.8 pg/mL (SD 3.2) at T−1 and 7.2 (SD 2.9) at T1 (p = 0.39) with a non-significant mean increase [0.4 pg/mL (SD 2.4; p = 0.12] (Fig. 1C).
We found an association between the level of CD4 count a T0 and the observed variations in humoral response from the peak after the 2nd dose (T−1) and 15 days after 3D (T1) (Fisher test p = 0.003). The difference was driven by the contrast between ICDR vs. HCDR (mean log2 0.5, std error 0.14, p = 0.002) (Supplementary Fig. 2A–C); in contrast, for the other two responses there was little evidence for an association with CD4 count: nAbs (fisher test p = 0.06) (Supplementary Fig. 3A–C) and for IFN-γ (p = 0.23) (Supplementary Fig. 4A–C).
Overall response to the third dose
The T1 values for anti-RBD were truncated for 30/216 (14%) at the cut off of 11,360 BAU/mL. The overall proportion of T1 value above the (log2 transformed) cut off of 7.1 BAU/mL was 214/216 (99%); three out of 4 (75%) participants in whom their anti-RBD level was <7.1 BAU/mL at T−1 showed a level above this cut-off post third dose.
In terms of the quantitative response in PLWH, the unadjusted anti-RBD IgG mean log2 were 7.3 BAU/mL (SD 2.8) at T0 and 11.8 (SD 2.2) at T1, (Fig. 2A). There was evidence for a significant increase from T0 to T1 (4.5 mean log2 (SD 1.9) [paired t-test (p < 0.0001)].
In HCWs, the unadjusted anti-RBD IgG mean log2 were 6.1 BAU/mL (SD 1.1) at T0 and 12.0 (SD 0.9) at T1, (Fig. 3A). There was evidence for a significant increase from T0 to T1 (5.9 mean log2 (SD 1.2) [paired t-test (p < 0.0001)].
Log2 change of anti-RBD IgG (A), MNA90 (B) and IFN-γ (C) from T0 to T1 in HCWs and PLWH; There was evidence for a significant increase of anti-RBD IgG, nAbs and IFN-γ from T0 to T1 (p < 0.0001, p < 0.0001 and p = 0.0015, respectively); (p-values are Bonferroni-corrected values). Green circles represent mean values of anti-RBD IgG, MNA900, and IFN-γ in HCWs, red circles represent mean values of anti RBD IgG, MNA90, and IFN-γ in PLWH. Source data are provided as a Source Data file.
If compared PLWH with the control group of HCWs and after adjusting for gender, age, and time difference in the exact day interval between the booster dose and the measured responses (between T0 and T1 and between T-1 and T0) we did not observe a difference of anti RBD at T1 between PLWH and HCWs [1.27 (−0.72, −3.27); p = 0.212] (Table 2).
The T1 values for nAbs were truncated for 107/216 (50%) at the cut off of 1:1280. The proportion of T1 value above the (log2 transformed) cut off of 1:10 was 206/216 (96%). Fourteen out of 20 (70%) participants in whom their nAbs level was < 1:10 at T−1 showed a level above this cut-off post third dose.
Regarding the quantitative response in PLWH, the unadjusted nAbs titres mean log2 were 4.9 (SD 2.1) at T0 and 8.7 (SD 2.1) at T1, (Fig. 2B). There was evidence for a significant increase from T0 to T1 (3.7 mean log2 (SD 2.2) [paired t-test (p < 0.0001)].
In HCWs, the unadjusted nAbs titres mean log2 were 3.4 (SD 1.4) at T0 and 7.9 (SD 1.3) at T1, (Fig. 3B). There was not a significant increase from T0 to T1 [4.6 mean log2 (SD 1.7); paired t-test (p < 0.0001)].
If compared PLWH with the control group of HCWs and after adjusting for gender, age and difference in the exact days interval between the booster dose and the measured responses (between T0 and T1 and between T−1 and T0) we did not observe a difference for nAbs at T1 PLWH and HCWs [1.24 (−1.37, 3.85);p = 0.353] (Table 2).
The overall proportion of T1 value above the (log2 transformed) cut off of 12 pg/mL was 186/216 (86%); only 4 out of 11 (36%) participants in whom their IFN-γ level was <12 pg/mL at T−1 showed a level above this cut-off post third dose.
Concerning the quantitative response in PLWH, the unadjusted IFN-γ mean log2 were 6.6 pg/mL (SD 3.5) at T0 and 7.36 (SD 2.9) at T1 (Fig. 2C). There was evidence for a significant increase from T0 to T1 (0.8 mean log2 (SD 3.0) [paired t-test (p = 0.003)].
In HCWs, the unadjusted IFN-γ mean log2 were 7.7 pg/mL (SD 1.8) at T0 and 8.7 (SD 1.7) at T1 (Fig. 3C). There was evidence for a significant increase from T0 to T1 (0.7 mean log2 (SD 3.0) [paired t-test (p = 0.0015)].
If compared with the control group of HCWs and after adjusting for gender, age and difference in the exact days interval between the booster dose and the measured responses (between T0 and T1 and between T-1 and T0) we observed a significant lower mean difference for IFN-γ at T1 in PLWH [−4.98 (−8.52, −1.44); p = 0.006] than HCWs (Table 2).
In terms of the qualitative response, 15 days after the third dose, anti-RBD-binding IgG response (>7.1 BAU/mL) was elicited in 95.5% of PCDR, 100% of ICDR, 100% of HCDR (Fisher exact test p = 0.04).
Only 2 participants (both in PCDR) did not show anti-RBD response < 7.1 BAU/mL and because of the small number of events, it was not possible to estimate the odds ratio according to the CD4 count strata.
In contrast, there was no evidence for a difference in the average increase by CD4 count strata by multivariable ANOVA (Fisher test p = 0.15) (Fig. 4A–C).
A−C Log2 change of anti-RBD IgG from T0 to T1 according to immunodeficiency status: PCDR (A), ICDR (B), HCDR (C). D−F Log2 increase of nAbs (MNA90) from T0 to T1 according to immunodeficiency status: PCDR (D), ICDR (E), HCDR (F). G−I Log2 increase of IFN-γ from T0 to T1 according to immunodeficiency status: PCDR (G), ICDR (H), HCDR (I) (ANOVA, 2-sided with Bonferroni adjusted p-values for multiple comparisons). Red dots represent mean values of anti RBD IgG, MNA90 and IFN-γ before the third dose, red squares represent mean values of anti RBD IgG, MNA90 and IFN-γ weeks after the third dose in PCDR; green dots represent mean values of anti RBD IgG, MNA90 and IFN-γ before the third dose, green squares represent mean values of anti RBD IgG, MNA90 and IFN-γ 2 weeks after the third dose in ICDR; Blue dots represent mean values of anti RBD IgG, MNA90 and IFN-γ before the third dose, blue squares represent mean values of anti RBD, MNA90 and IFN-γ 2 weeks after the third dose IN HCDR. Source data are provided as a Source Data file.
Specifically, the unadjusted anti-RBD IgG mean log2 were 5.1 BAU/mL (SD 3.7) at T0 and 10 (SD 3.7) at T1 in PDCR, 7.4 BAU/mL (SD 2.4) at T0 and 12.1 (SD 1.5) at T1 in HCDR and 8.4 BAU/mL (SD 1.7) at T0 and 12.3 (SD 1.2) at T1 with no significant differences among groups (Fisher test, p = 0.19).
The results from the truncated linear regression analysis carried no evidence for an overall effect of CD4 count on RBD-binding IgG (global Wald test p = 0.20) (Table 3).
Mean variations over T0–T1 of anti-RBD IgG levels after the third dose according to CD4 count strata are shown in Supplementary Fig. 5A.
Only one participant with anti-RBD IgG level < 7 BAU/mL was found and he/she received all three doses with BNT162b2 vaccination group.
The mean log2 increase of anti-RBD IgG comparing T0 to T1 according to vaccine sequence were: 4.5 (SD 2.1) in BNT162b2 group, 4.0 (1.4) in mRNA-1273 group, 5.9 (1.7) in 2BNT162b2 + mRNA-1273 group and 3.3 (1.6) in 2mRNA-1273 + BNT162b2 group (Fisher p < 0.0001 in the age-adjusted ANOVA); there was evidence for a difference for four individual contrasts: 2BNT162b2 + mRNA-1273 vs. mRNA-1273 group (mean log2 difference 0.95, std error 0.15; Bonferroni-corrected p < 0.0001), 2BNT162b2 + mRNA-1273 vs. 2mRNA-1273 + BNT162b2 (1.30, std error 0.19; p < 0.0001), 2BNT162b2 + mRNA-1273 vs. BNT162b2 (0.69, std error 0.17; p = 0.004) and finally 2mRNA-1273 + BNT162b2 vs. BNT162b2 (0.61, std error 0.20; p = 0.02) (Supplementary Fig. 6A).
The results from the truncated linear regression analysis confirmed an overall association with vaccine sequence strata (global Wald test p = 0.0007) and a significant difference for all four individual contrasts (see below).
In terms of the qualitative response, 15 days after the third dose, nAbs (defined as titres > 1:10) was elicited in 86.3% of PCDR, 97.9% of ICDR, 98.7% of HCDR (Fisher exact p = 0.001). In the multivariable logistic regression model, using HCDR as the comparator, PCDR showed a largely increased risk of failing to achieve nAbs > 1:10, after adjusting for the main identified confounders (age, time from HIV diagnosis, CD4 nadir, HIV-RNA < 50 vs > 50 copies/mL at the time of third dose, days from the date of 2nd dose, vaccine sequence and concomitant cancer), although not statistically significant [aOR 5.04 (95% CI 0.22, 115.1); p = 0.31] (Table 2). Similarly, there was no evidence for a difference in the average increase by CD4 count strata by multivariable ANOVA (Fisher p = 0.41) (Fig. 3D–F). Mean delta changes of nAbs titres after the third dose according to CD4 count strata are shown in Supplementary Fig. 5B. Specifically, the unadjusted nAbs mean log2 were 3.7 (SD 2.2) at T0 and 7.3 (SD 2.9) at T1 in PDCR, 5.1 (SD 2.1) at T0 and 9.0 (SD 1.9) at T1 in HCDR and 5.7 (SD 1.8) at T0 and 9.1 (SD 1.5) at T1 with no significant differences among groups (Fisher test, p = 0.18).
Similarly, the truncated linear regression analysis did not show an overall association both with CD4 count strata and magnitude of nAbs(global Wald p = 0.26) (Table 3) and risk of non response to the third dose (Table 4).
Finally, the mean log2 increase of nAbs comparing T0 to T1 according to vaccine sequence were: 4.09 (SD 2.57) in BNT162b2 group, 3.32 (1.98) in mRNA-1273 group, 4.59 (2.02) in 2BNT162b2 + mRNA-1273 group and 2.77 (1.85) in 2mRNA-1273 + BNT162b2 (age-adjusted ANOVA F p = 0.0003); there was evidence for a difference for three contrasts: 2BNT162b2 + mRNA-1273vs. mRNA-1273 group (mean log difference 0.63, std error 0.18; p = 0.0006), HtM vs. HtP (0.91, std error 0.23; p = 0.0001), and BNT162b2 group vs. 2mRNA-1273 + BNT162b2 (0.65, std error 0.24; p = 0.008) (Supplementary Fig. 6B). The results from the truncated linear regression analysis confirmed an overall association with vaccine sequence strata (global Wald test p < 0.0001) and a significant difference for all individual contrasts (Table 5).
In terms of the qualitative response, IFN-γ (defined as levels >12 pg/mL) was elicited in 70% of PCDR, 95.7% of ICDR, 97.2% of HCDR (chi-square p < 0.0001).
There was no evidence for a difference in the average increase by CD4 count strata by multivariable ANOVA (Fisher p = 0.23) (Table 3 and Fig. 4G–I). Mean delta changes of IFN-γ levels after the third dose according to CD4 count strata are shown in Supplementary Fig. 5C.
Specifically, the unadjusted IFN-γ mean log2 were 4 pg/mL (SD 3.6) at T0 and 4.7 (SD 3.7) at T1 in PDCR, 7 (SD 3.2) at T0 and 7.7 (SD 2.2) at T1 in HCDR and 7.4 (SD 3.3) at T0 and 8.5 (SD 2.2) at T1 with no significant differences among groups (Fisher test, p = 0.87).
In the multivariable logistic regression model using HCDR as the comparator, PCDR showed and increased risk of failing to achieve IFN-γ > 12 pg/mL, after adjusting for the main identified confounders (age, time from HIV diagnosis, CD4 nadir, HIV-RNA at the time of third dose, days from the date of 2nd dose, vaccine sequence and concomitant cancer), although not statistically significant [2.48 (0.29, 21.56); p = 0.41] (Table 4).
The mean log2 increase of IFN- γ comparing T0 to T1 according to vaccine sequence were: 0.47 (SD 3.79) in BNT162b2 group, 0.96 (3.09) in mRNA-1273 group, 0.72 (2.36) in 2BNT162b2 + mRNA-1273 and 0.74 (2.55) in 2mRNA-1273 + BNT162b2, with no evidence for a difference between the groups (age adjusted p = 0.92, Supplementary Fig. 6C; Table 5).
Participants were asked to report side-effects in days 0−7 after the third dose and overall 68% (146/216) of them reported at least one symptom. Among them, 95% reported mild symptoms, 14% moderate symptoms, and 2% severe symptoms not requiring hospitalization. Specifically, 82% complained about inoculation site pain, 44% fatigue, 38% myalgia, 37% fever, 25% headache, 23% shivering and 15% swelling; other symptoms less frequently reported were rash, cough, sore throat, rhinorrhoea, heavy breathing, nausea, vomit or diarrhea which were overall reported by 30.8% of the participants (Fig. 5). The data carried no evidence for a difference in the prevalence of reported side-effects according to CD4 count strata with the only exception of shivering which was more frequently reported in HCDR (37% vs 19% in ICDR and 13% in PCDR; p = 0.023).
The side-effects frequency distribution according to vaccine sequence groups showed that 2BNT162b2 + mRNA-1273 group experienced a higher proportion of symptoms as compared to other combinations (Supplementary Fig. 7).
Discussion
In this analysis, we found that a third dose of mRNA anti-SARS-CoV-2 vaccine induced a strong humoral and T specific cell response in PLWH eligible for third dose who previously received a complete mRNA 2-dose vaccination cycle. Interestingly, anti RBD IgG, neutralizing antibodies and T cell-mediated response all showed a significant increase. Of note, the level of anti RBD IgG, neutralizing antibodies achieved after the third dose was even higher than that observed one month after the 2nd dose of the primary cycle. Although no significant association could be found with the current level of CD4 count, our data cannot rule out a difference in both the magnitude of response and risk of no-response when comparing participants with poor CD4 count recovery on ART (PCDR) with those high CD4 count recovery on ART (HCDR). Conversely, the level of T cell mediated response appeared to be more stable comparing values achieved post 2nd dose with those observed post the third dose.
The comparison with a HIV negative control group (HCWs) did not show significantly different anti-RBD and nAbs responses. In contrast, the data carried significant evidence for a lower mean difference in IFN-gamma between PLWH and controls. Thus, these are important results as they show that despite a significant response to a third dose, PLWH appear to have an impaired T-cell mediated response as compared to the general population.
These findings are in line with that recently observed on the characterization of the humoral and SARS-CoV-2 T-cell specific response in PLWH following a mild COVID19, which seem comparable between HIV positive and HIV negative subjects. Moreover, we found a significant difference in term of T-cell specific response in PLWH which results lower than that observed in HIV negative control group and we argue that the overall magnitude of SARS-CoV-2-specific T cell responses relates to the size of the naive CD4 T cell pool, suggesting that inadequate immune reconstitution on ART, could hinder immune responses to SARS-CoV-2 and vaccine effectiveness in PLWH28.
The observed increase in humoral response in our setting is also consistent with the hypothesis that third dose induces a robust B cell memory response29, previously elicited by the primary vaccination series and highlights the fact that the SARS-CoV-2 mRNA vaccines are able to stimulate a satisfactory humoral response even in immunocompromised patients such as those with low CD4 count and a previous or current diagnosis of AIDS. These data could be relevant as they add new insights on immune response to supplemental mRNA vaccine in PLWH.
Recently, a matched case-control on humoral response to primary mRNA vaccination cycle in HIV positive and HIV negative showed that PLWH had lower surrogate virus neutralization test response and a trend towards lower IgG response, particularly among those with lower CD4 + T-cell counts and who received the BNT162b2 vaccine (vs mRNA1273), highlighting the need to identify groups that have reduced response to SARS-CoV-2 vaccination in order to set an optimal vaccination schedule with a third additional dose30.
These response rates are remarkable if compared with those observed in other immunocompromised patients. The rate of anti-RBD response after a third dose in individuals with chronic lymphocytic leukemia (CLL) was of 72% and was even lower when restricting to patients on chemoimmunotherapy (60%)31. In non- or low-responders on hemodialysis to standard vaccination, a third dose was able to induce effective antibody titres in only about 70% of patients32.
However, our findings are comparable with the results of a recent report on immunogenicity in individuals with hematologic and solid cancers33, and in another study an immediate antibody response to booster administration of theBNT162b2 vaccine was observed in almost all patients with solid organ tumors, including those receiving active systemic chemotherapy34.
Both the primary vaccination cycle and the third dose were able to increase the Spike-specific T cell response. Nevertheless, differently from the antibody production, the T cell response elicited by the third dose was similar than that achieved by the primary vaccination cycle, suggesting that a fully T-cell immunization is still achieved with the first two doses. The T cell response that contracted overtime after the first two doses can be effectively boosted by the additional third dose. Most of our PLWH with severe immunodeficiency at the time of their first vaccine dose showed an anti-RBD IgG response (95.5%), nAbs response (86.3%) and T cell immunity (70%) after the third dose, and these figures appear to be remarkable in the light of the severe and persistent immunologic dysregulation in this population, due to a reduced T and B cell functionality induced by residual inflammation and immune-senescence processes35. The achieved responses are particularly impressive, considering the participants’ status of chronic immune dysregulation, as well as the fact that depletion of viral-specific T and B cell clones is observed even in PLWH responder to antiretroviral therapy (cART)36,37. Despite the fact that cART durably leads to HIV-RNA suppression and CD4 + T-cell restoration, and reverses HIV related immune dysfunction38,39 a persistent immunopathology, as that observed in HIV chronic disease, can weaken the general immune responses to vaccination40,41. Our cohort of advanced PLWH previously stimulated by a full cycle vaccination showed an optimal response to a third dose. This finding seems to imply that effective cART is able to both inhibit HIV replication and to restore a good immune response, also in patients with low CD4 count or who experienced AIDS events. However, the impact of HIV-related immunosuppression on the duration of the vaccine-induced immunity still remains to be fully elucidated. Indeed, it has been reported that the CD4 count is the earliest and critical driver in orchestrating an optimal vaccine induced immune response28,30,41. In chronic PLWH, the CD4 T cells as well as the persistent low inflammatory environment could dampen the differentiation of effective and long-lived memory B and T cell immunity42,43. Although overall the data carried little evidence for an association between current level of CD4 count and response to vaccine, we found a significant difference in humoral response when comparing participants with poor CD4 count recovery on ART (PCDR) with those having a high CD4 count recovery (HCDR). Also for the other responses there was a tendency for those with PCDR to show worse outcomes then those having HCDR, although results were not significant likely because of low statistical power. Further studies are mandatory to address this point, which is key to better design the future vaccination schedules in PLWH.
Our study also strongly supports a difference in terms of humoral response to the third dose depending of the type of vaccine sequence received: participants who received as primary series BNT162b2 followed by a third dose with mRNA-1273 showed a higher mean increase of humoral response than those received other sequences. Although formal conclusions regarding the clinical significance of this observed difference cannot be made, our data are consistent with the results of another recent study showing higher immunogenicity and significantly enhanced effectiveness of two doses of mRNA1273 compared with BNT162b244,45 and with the hypothesis that the observed higher vaccine response with the mRNA-1273 could be related to the additional week between administrations, higher vaccine dose, differences in inducing T cell subsets, or other factors30.
Further, a blinded, multicenter, randomized, controlled, phase 2 trial performed in the UK (the COV-BOOST study), have shown that among the type of vaccine typically used as booster dose after a primary cycle with BNT162b2, mRNA127 was the type of vaccine able to elicit the highest titres of anti-Spike IgG, neutralizing wild type virus antibodies and cellular immunity, with comparable results regardless of age46.
Our analysis also provides indirect evidence that the strong neutralizing activity achieved with a third dose may reduce the risk of infection with emerging VoC, such as the Omicron variant. Indeed, recent in vitro studies have demonstrated that higher level of nAbs titres, enhancing a cross reactivity of antibody response, are needed to neutralize Omicron, which could be obtained by deploying third booster doses of vaccine8,9,10,11,47. A mRNA third dose seems to enhance overall levels of anti-SARS-CoV-2 neutralizing antibodies, above a threshold allowing inhibition of Omicron13, even though the waning of this immune response has not been yet fully recognized10.
Moreover, the T cell response induced by both vaccination and natural infection has been shown able to efficiently recognize the Omicron variant (70−80% of CD4 and CD8 T cells cross-recognize Omicron), thus contributing to the protection from severe COVID-19. Therefore, the vaccination in PLWH could significantly reduce the risk of severe Omicron disease by increasing the titer of neutralizing antibody and by inducing an efficient and cross-reactive T cell response48,49.
Finally, the safety profiles after the additional injection were generally similar to those observed after the primary series and reported in the previously reported phase 2 and 3 clinical trials50,51,52. The most common local side effect was pain in the inoculation site while, among systemic events after the third dose, were fatigue, headache, myalgia and fever which occurred at similar frequencies. These frequencies are similar to those reported in randomized trials although the COV-BOOST trial estimates are significantly higher for those who received as primary series BNT162b2 and for booster dose mRNA-127346.
To our knowledge, ours is the first analysis to characterize the immune response and reactogenicity to a third dose of SARS-CoV-2 vaccination in PLWH, and to provide quantification estimates of the level of immunogenicity elicited by an additional boosting dose in PLWH, particularly in those with advanced immune dysregulation. Our data also documents how the level of response may differ by mRNA COVID-19 vaccines administered as third dose according to the primary cycle used and which sequence has the best chance to boost serologic, neutralizing and cell-mediated response in this vulnerable population.
The main limitation of our analysis is the observational, not randomized nature of the study design, so that uncontrolled sources of unmeasured confounding bias (e.g. socio-economic factors) may exist16. Despite the prospective design and the careful methodological evaluation, causal links are difficult to establish in this setting. This is particularly true for the association between CD4 count at T0 and the variation in response between T-1 and T1 because the evaluation of the exposure does not strictly precede the outcome. The high proportion of participants with a truncated value for anti-RBD and nAbs responses at T1 also further complicated the interpretation of the results for these outcomes.
Also, the definition of the binary outcome for the T-cell response was based on a non-standardized threshold and because of the small number of events observed especially in the ICDR and HCDR groups, the evaluation of the association with current CD4 count with all binary endpoints was likely to be underpowered.
Moreover, the present analysis concerns only the short term response (up to 15 days after the 3D) and therefore we were unable to provide estimates of the durability of immune response and waning of immunogenicity after a third dose in PLWH.
A further limitation is the fact that clinical outcome such as the rate of infection and of disease severity was not evaluated so we were unable to establish whether the increased level of immunogenicity was associated also with a reduced incidence of these clinical events. Although the concept is supported by in vitro data and by studies conducted in the general population3,4,5,6,7,8,9,10,11, whether the high level of nAbs elicited by the third dose in our population is able to reduce the risk of infection with newly circulating VoC such as Omicron remains to be seen.
Despite these limitations, the findings presented here indicate that in PLWH with advanced disease at the time of their first vaccination dose, providing an additional dose of SARS-CoV-2 mRNA vaccine at least 4 months after the initial two-dose vaccination, resulted in markedly higher levels of boosted immunity after initial course. Although the clinical effectiveness of the third dose has to be definitively proven by further and larger studies, these early data appears to support the decision to provide a short term third dose to this subset of PLWH.
Methods
Study design and population
On September 10th, 2021, as part of the Nationwide Booster Vaccination Program in Italy, the National Institute for Infectious Diseases Lazzaro Spallanzani in Rome started the boosting vaccination against SARS-CoV-2 in PLWH, as a third dose of a mRNA vaccine (a full additional dose of BNT162b2 or mRNA-1273), according to the Italian Ministry of Health recommendations, for those who, at the time of their first vaccine dose showed a CD4 < 200/mm3 or were previously diagnosed with AIDS.
Participants in this analysis are a subset of those who, following written informed consent, had been enrolled in an observational cohort study to evaluate the outcomes of SARS-CoV-2 vaccination (the HIV-VAC study). HIV-VAC was approved by the Scientific Committee of the Italian Drug Agency (AIFA) and by the Ethical Committee of the Lazzaro Spallanzani Institute, as National Review Board for COVID-19 pandemic in Italy (approval number 423/2021). Details of this study have been described elsewhere27.
Specifically, the present analysis includes PLWH consecutively enrolled in HIV-VAC for whom in October 20th, 2021 there was at least a 28 days gap after having completed the 2-dose schedule with BNT162b2 or mRNA-1273 vaccines, and receiving a third dose. Individuals with a SARS-CoV-2 infection diagnosis, defined by a RT-PCR positive to the molecular test on the nasopharyngeal swab, or positivity to anti-N IgG at T0, were excluded for the present analysis.
Participants’ demographic, epidemiologic, clinical and laboratory characteristics at time of the third dose were collected. Exact vaccine sequence was recorded. Also, humoral and neutralizing antibodies responses were retrospectively measured in blood samples which were stored at time of third dose (T0) and approximately 15 days after the third dose (T1). T-cell response was measured on fresh blood collected at the same times. In addition, both humoral neutralizing antibodies and T-cell responses measured approximately 30 days after participants’ second vaccine dose were also available for comparative analysis (time T-1). In addition, at day 7 after the third dose, participants were asked via a telephone interview about solicited adverse events which might have occurred over the period 0−7 days following the third dose. Finally, ninety-eight HIV seronegative health care workers (HCWs) were included for comparison, from whom samples were collected before and after the booster dose (to be intended as a booster dose, a full dose of BNT162b2 or half a dose of mRNA-1273).
Laboratory procedures
Two commercial chemiluminescence microparticle antibody assays (CMIA), the SARS-CoV-2 specific anti-N, and the anti-S/RBD tests (ARCHITECT SARS-CoV-2 IgG, and ARCHITECT SARS-CoV-2 IgG II Quantitative, Abbott Laboratories, Wiesbaden, Germany respectively,) were performed on ARCHITECT® i2000sr (Abbott Diagnostics, Chicago, IL, USA) and used according to manufacturer’s instruction; Index >1.4 and Binding Antibody Units (BAU)/mL ≥ 7.1 are considered positive, respectively.
Micro-neutralization assay (MNA) was performed using SARS-CoV-2/Human/ITA/PAVIA10734/2020, as challenging virus16. Briefly, serum samples were heat-inactivated at 56 °C for 30 min, and titrated in duplicate in 7 two-fold serial dilutions (ranging from 1:10 to 1:640). Equal volumes (50 μL) of serum and medium containing 100 tissue culture infectious doses 50% (TCID50) SARS-CoV-2 were mixed and incubated at 37 °C for 30 min. Serum-Virus mixtures were then added to sub-confluent Vero E6 cell (ATCC, Manassas, Virginia, United States, CRL-1586™) monolayers and incubated at 37 °C and 5% CO2. After 48 h, microplates were observed by light microscope for the presence of cytopathic effect (CPE). To standardize inter-assay procedures, positive control samples showing high (1:160) and low (1:40) neutralizing activity were included in each assay session. Serum from the National Institute for Biological Standards and Control, UK (NIBSC) with known neutralization titer (Research reagent for anti-SARS-CoV-2 Ab NIBSC code 20/136) was used as reference in MNA. The standardized cut off of MNA90 ≥ 1:10 was used to define neutralization activity; only for computational and statistical purposes, samples resulted > = 1:640 were arbitrarily considered =1:1280.
We studied IFN-γ production in response to Spike stimulation as a surrogate of specific T-cell function. Peripheral blood was collected in heparin tubes and stimulated or not with a pool of peptides spanning the Spike protein (Miltenyi Biotech, Germany) at 37 °C (5% CO2). A superantigen (SEB) was used as positive control. Plasma were harvested after 16-20 hours of stimulation and stored at −80 °C. IFN-γ released in plasma after stimulation was quantified using an automated ELISA (ELLA, Protein Simple). The detection limit of these assays was 0.17 pg/mL for IFN-γ and the cut off used in this analysis to define the T-specific cells response was 12 pg/mL, calculated as the mean + 2 SD of the response to spike peptides of unvaccinated uninfected heathy donors53.
Statistical analysis
The primary outcome was immunogenicity (humoral, neutralizing and cell-mediated responses) measured 15 days after receiving the third dose (T1). This was defined as both quantitative/continuous (average difference between T0 and T1) or qualitative/binary (lack of response). The latter outcomes were immunogenic parameter specific which were defined as follows: anti-RBD IgG Binding Antibody Units <7.1 (BAU)/mL, MNA90 < 1:10 and for IFN-γ < 12 pg/mL. Secondary outcomes were i) 0−7 days reactogenicity (self-reported by telephone interview), and ii) the difference in average level of immunogenicity between T−1 and T1.
Because the distribution of the immunogenic response parameters was positively skewed, a log2 transformation was used for all measures (RBD-binding IgG, nAb titres, IFN-γ), to make the data conform more closely to the normal distribution and to improve the model fit.
Mean and standard deviation in the log2 scale are presented and a paired t-test was used to test a difference from zero in the overall changes over T0–T1.
Participants were then stratified by CD4 count at T0 in three groups according to the size of CD4 count recovery: CD4 count <200 cell/mm3: poor CD4 recovery (PCDR); CD4 count between 200 and 500 cell/mm3: intermediate CD4 recovery (ICDR); CD4 count >500 cell/mm3: high CD4 recovery (HCDR) and according to vaccine sequence: i) primary series with BNT162b2, third dose with BNT162b2 (BNT162b2 group); ii) primary series with mRNA-1273, third dose with mRNA-1273 (mRNA-1273 group); iii) primary series with BNT162b2, third dose with mRNA-1273 (2BNT162b2 + mRNA-1273 group); iv) primary series with mRNA-1273, third dose with BNT162b2 (2mRNA-1273 + BNT162b2). Strata specific mean values of RBD-binding IgG, nAb titres, IFN-γ with standard deviations were also shown.
Proportions of participants who failed to achieve a level of immunogenicity above the thresholds described above were calculated by CD4 count and vaccine sequence strata and compared using a chi-square or Fisher exact test as appropriate. ANOVA, logistic regression models and truncated regression models were used to evaluate the association between these two exposure factors (current CD4 count and vaccine sequence) and the level of immunogenic response.
In the ANOVA analysis we used the naïve approach of replacing the truncated values with the upper limit of the assay for anti-RBD > 7.1 BAU/mL and nAbs > 1:10). When comparing mean responses by ANOVA, after checking that an overall difference between the groups existed, specific pairwise contrasts hypothesis testing was performed, after controlling for the inflation of type I error due to multiple testing. Specifically, Dunn’s test with Bonferroni correction was used to adjust the p-values of these pairwise contrasts.
Univariable and multivariable regression models were fitted (logistic and truncated regression). For the logistic regression the binary outcome was lack of immunogenic response as defined above. Because of the large number of participants with a response value above the upper limit cut-off of the assay, ANOVA results could be biased. Truncated linear regression adequately controlled for censored data for the outcome variable, it was similar to ANOVA but was fitted on the natural scale of the responses and correctly accounted for truncated values (participants who reached the upper limit of the assay for specific responses).
When CD4 count at T0 was the exposure of interest, the following variables have been identified as potential confounders for the association between CD4 count and immunogenic responses: age, time from HIV diagnosis, CD4 nadir, HIV-RNA at the time of third dose, days from the date of 2nd dose, vaccine sequence and concomitant cancer. These model assumptions are described by means of a direct acyclic graph (DAG), built using DAGitty vers. 2.3 released 2015-08-19, available at http://www.daggity.net/ (Supplementary Fig. 1). Because vaccine sequence allocation was pseudo-random, only age-adjusted models have been used to evaluate the association between this factor and immunogenic response.
Furthermore, we performed an additional analysis of covariance analysis with the aim to compare humoral and SARS-CoV-2 T-cell specific between our cohort of PLWH and health care workers (HCWs) after controlling for gender, age and time difference in the exact day intervals between the booster dose and the measured response (between T0 and T1 and between T-1 and T0).
A descriptive analysis of the secondary outcome measuring self-reported side effects was also performed showing the proportion of participants reporting specific side effects by CD4 count and vaccine sequence strata. Chi-square test was used to compare these proportions.
All statistical analyses were performed using SAS Statistical Software v.9.4 (SAS Institute Inc., Carey, NC, USA). All figures were generated using GraphPad Prism 9.0 (GraphPad Software, Inc., San Diego, CA).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The HIV-VAC data are available under restricted access for confidentiality reasons, since these patients may be identified by combinations of person-specific characteristics within the database; access can be obtained by specific request to the corresponding author. The raw data on demographics and clinical status of participants, are protected and not available due to data privacy laws. The processed data are available by specific request to alessandra.vergori@inmi.it. Source data are provided with this paper.
References
WHO Coronavirus (COVID19) Dashboard. Available at: https://covid19.who.int.
Koff, W. C. et al. Development and deployment of COVID-19 vaccines for those most vulnerable. Sci. Transl. Med. 13, eabd1525 (2021). PMID: 33536277.
Lopez Bernal, J. et al. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 385, 585–594 (2021). Epub 2021 Jul 21. PMID: 34289274; PMCID: PMC8314739.
Nasreen, S. et al. Effectiveness of COVID-19 vaccines against variants of concern in Ontario, Canada. medRxiv. 06.28.21259420; https://doi.org/10.1101/2021.06.28.21259420. (2021)
Comirnaty and Spikevax: EMA recommendations on extra doses and boosters. Available at: https://www.ema.europa.eu/en/news/comirnaty-spikevax-ema-recommendations-extra-doses-boosters.
CDC Expands COVID-19 Booster Recommendations. https://www.cdc.gov/media/releases/2021/s1129-booster-recommendations.html.
Choi, A. et al. Safety and immunogenicity of SARS-CoV-2 variant mRNA vaccine boosters in healthy adults: an interim analysis. Nat. Med. https://doi.org/10.1038/s41591-021-01527-y. (2021) Epub ahead of print. PMID: 34526698.
Meng, B. et al. CITIID-NIHR BioResource COVID-19 Collaboration, The Genotype to Phenotype Japan(G2P-Japan) Consortium, Choi J, Lee JH, Mlcochova P, James L, Doffinger R, Thukral R, Sato K, Gupta RK. SARS CoV-2 Omicron spike mediated immune escape, infectivity and cell-cell fusion. bioRxiv; https://doi.org/10.1101/2021.12.17.473248.
Dejnirattisai, W. et al. Com-COV2 Study Group. Reduced neutralization of SARS-COV-2 Omicron-B.1.1.529 variant by post-immunisation serum. medRxiv preprint https://doi.org/10.1101/2021.12.10.21267534.
Planas, D. et al. Considerable escape of SARS-CoV-2 variant Omicron to antibody neutralization. bioRxiv preprint https://doi.org/10.1101/2021.12.14.472630; this version posted December 15, 2021.
Garcia-Beltran, W. F. et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell, 2021; PII: S0092-8674(21)01496-3; https://doi.org/10.1016/j.cell.2021.12.033.
Geretti, A. M. et al. Outcomes of Coronavirus Disease 2019 (COVID-19) Related Hospitalization Among People With Human Immunodeficiency Virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): A Prospective Observational Study. Clin. Infect. Dis. 73, e2095–e2106 (2021). PMID: 33095853; PMCID: PMC7665382.
Bhaskaran, K. et al. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Hiv. 8, e24–e32 (2021). Epub 2020 Dec 11. PMID: 33316211; PMCID: PMC7773630.
Tesoriero, J. M. et al. COVID-19 Outcomes Among Persons Living With or Without Diagnosed HIV Infection in New York State. JAMA Netw. Open. 4, e2037069 (2021). PMID: 33533933; PMCID: PMC7859843.
Spinelli, M. A. et al. SARS-CoV-2 seroprevalence, and IgG concentration and pseudovirus neutralization antibody titres after infection, compared by HIV status: a matched case-control observational study. Lancet HIV. 20218:e334-e341. Epub 2021 Apr 29. PMID: 33933189; PMCID: PMC8084354.
Fehr, D. et al. Characterization of people living with HIV in a Montreal-based tertiary care center with COVID-19 during the first wave of the pandemic. AIDS Care. 20211-7. https://doi.org/10.1080/09540121.2021.1904500. Epub ahead of print. PMID: 33779425.
Sheth, A. N., Althoff, K. N. & Brooks, J. T. Influenza susceptibility, severity, and shedding in HIV-infected adults: a review of the literature. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 52, 219–227 (2011).
Frater, J. et al. Oxford COVID Vaccine Trial Group. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: a single-arm substudy of a phase 2/3 clinical trial. Lancet Hiv. 8, e474–e485 (2021). Epub 2021 Jun 18. PMID: 34153264; PMCID: PMC8213361.
Ogbe, A. et al. Durability of ChAdOx1 nCov-19 (AZD1222) vaccination in people living with HIV – responses to SARS-CoV-2, variants of concern and circulating coronaviruses. medRxiv 2021.09.28.21264207; https://doi.org/10.1101/2021.09.28.21264207
Levy, I. et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in people living with HIV-1. Clin. Microbiol Infect. 27, 1851–1855 (2021). Epub 2021 Aug 24. PMID: 34438069; PMCID: PMC8382485.
Woldemeskel, B. A. et al. The BNT162b2 mRNA Vaccine Elicits Robust Humoral and Cellular Immune Responses in People Living with HIV. Clin Infect Dis. (2021)ciab648. https://doi.org/10.1093/cid/ciab648. Epub ahead of print. PMID: 34293114; PMCID: PMC8406881.
Ruddy, J. A. et al. Safety and antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in persons with HIV. AIDS 35, 2399–2401 (2021). PMID: 34261097.
Brumme, Z. L. et al. Humoral immune responses to COVID-19 vaccination in people living with HIV receiving suppressive antiretroviral therapy. medRxiv [Preprint]. 20212021.10.03.21264320. https://doi.org/10.1101/2021.10.03.21264320. PMID: 34671779; PMCID: PMC8528088.
Lombardi, A. et al. Anti-spike antibodies and neutralization antibody activity in people living with HIV vaccinated with COVID-19 mRNA-1273 vaccine: a prospective single centre cohort study. The Lancet Regional Health – Europe, Volume 0, Issue 0, 100287.
Aledo, M. G. et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 and BNT162b2 vaccines in people living with HIV. AIDS. https://doi.org/10.1097/QAD.0000000000003161. (2022) Epub ahead of print. PMID: 34999608.
Jedicke, N. et al. Humoral immune response following prime and boost BNT162b2 vaccination in people living with HIV on antiretroviral therapy. HIV Med. https://doi.org/10.1111/hiv.13202. (2021) Epub ahead of print. PMID: 34725907; PMCID: PMC8652991.
Antinori, A. et al. HIV-VAC Study Group. Humoral and cellular immune response elicited by mRNA vaccination against SARS-CoV-2 in people living with HIV (PLWH) receiving antiretroviral therapy (ART) according with current CD4 T-lymphocyte count. Clin Infect Dis. ciac238. https://doi.org/10.1093/cid/ciac238. (2022) Epub ahead of print. PMID: 35366316.
Alrubayyi, A. et al. Characterization of humoral and SARS-CoV-2 specific T cell responses in people living with HIV. Nat. Commun. 12, 5839 (2021).
Turner, J. S. et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 596, 109–113 (2021). Epub 2021 Jun 28. PMID: 34182569.
Spinelli, M. A. et al. Differences in Post-mRNA Vaccination SARS-CoV-2 IgG Concentrations and Surrogate Virus Neutralization Test Response by HIV Status and Type of Vaccine: a Matched Case-Control Observational Study. Clin. Infect. Dis. ciab1009. https://doi.org/10.1093/cid/ciab1009. (2021) Epub ahead of print. PMID: 34864962; PMCID: PMC8689738.
Bagacean, C. et al. Humoral response to mRNA anti-COVID-19 vaccines BNT162b2 and mRNA-1273 in patients with chronic lymphocytic leukemia. Blood Adv. bloodadvances.2021006215. https://doi.org/10.1182/bloodadvances.2021006215. (2021) Epub ahead of print. PMID: 34844264.
Tillmann, F. P. et al. P. Evolution of SARS-CoV-2-Neutralizing Antibodies after Two Standard Dose Vaccinations, Risk Factors for Non-Response and Effect of a Third Dose Booster Vaccination in Non-Responders on Hemodialysis: A Prospective Multi-Centre Cohort Study. J. Clin. Med. 10, 5113 (2021). PMID: 34768631; PMCID: PMC8584296.
Ehmsen, S. et al. Antibody responses following third mRNA COVID-19 vaccination in patients with cancer and potential timing of a fourth vaccination. Cancer Cell. S1535-6108(22)00063-0. https://doi.org/10.1016/j.ccell.2022.02.011. (2022) Epub ahead of print. PMID: 35216675; PMCID: PMC8867110.
Rottenberg, Y. et al. Assessment of Response to a Third Dose of the SARS-CoV-2 BNT162b2 mRNA Vaccine in Patients With Solid Tumors Undergoing Active Treatment. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2021.6764. (2021) Epub ahead of print. PMID: 34812840.
Deeks, S. G. HIV infection, inflammation, immunosenescence, and aging. Annu Rev. Med 62, 141–155 (2011). PMID: 21090961; PMCID: PMC3759035.
Plana, M. et al. Immunological benefits of antiretroviral therapy in very early stages of asymptomatic chronic HIV-1 infection. AIDS 14, 1921–1933 (2000). PMID: 10997396.
Kaufmann, G. R. et al. Rapid restoration of CD4 T cell subsets in subjects receiving antiretroviral therapy during primary HIV-1 infection. AIDS 14, 2643–2651 (2000). PMID: 11125882.
El Chaer, F. & El Sahly, H. M. Vaccination in the Adult Patient Infected with HIV: A Review of Vaccine Efficacy and Immunogenicity. Am. J. Med. 132, 437–446 (2019).
Kernéis, S. et al. Long-term immune responses to vaccination in HIV-infected patients: a systematic review and meta-analysis. Clin. Infect. Dis. 58, 1130–1139 (2014). Epub 2014 Jan 10. PMID: 24415637; PMCID: PMC4761378.
Geretti, A. M. & Doyle, T. Immunization for HIV-positive individuals. Curr. Opin. Infect. Dis. 23, 32–38 (2010).
Painter, M. M. et al. Rapid induction of antigen-specific CD4+ T cells is associated with coordinated humoral and cellular immunity to SARS-CoV-2 mRNA vaccination. Immunity 54, 2133–2142.e3 (2021). Epub 2021 Aug 13. PMID: 34453880; PMCID: PMC8361141.
Cain, D., Kondo, M., Chen, H. & Kelsoe, G. Effects of acute and chronic inflammation on B-cell development and differentiation. J. Invest Dermatol. 129, 266–277 (2009). PMID: 19148216; PMCID: PMC2778726.
Moro-García, M. A., Mayo, J. C., Sainz, R. M. & Alonso-Arias, R. Influence of Inflammation in the Process of T Lymphocyte Differentiation: Proliferative, Metabolic, and Oxidative Changes. Front. Immunol. https://doi.org/10.3389/fimmu.2018.00339. (2018)
Naranbhai, V. et al. Comparative immunogenicity and effectiveness of mRNA-1273, BNT162b2 and Ad26.COV2.S COVID-19 vaccines. medRxiv [Preprint]. 20212021.07.18.21260732. https://doi.org/10.1101/2021.07.18.21260732. PMID: 34671780; PMCID: PMC8528089.
Dickerman, B. A. et al. Comparative Effectiveness of BNT162b2 and mRNA-1273 Vaccines in U.S. Veterans. NEJM. https://doi.org/10.1056/NEJMoa2115463. (2021)
Munro, A. P. S. et al. COV-BOOST study group. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomized, controlled, phase 2 trial. Lancet. S0140-6736(21)02717-3. https://doi.org/10.1016/S0140-6736(21)02717-3. (2021) Epub ahead of print. PMID: 34863358.
Keeton, R. et al. SARS-CoV-2 spike T cell responses induced upon vaccination or infection remain robust against Omicron. MedRxiv. https://doi.org/10.1101/2021.12.26.21268380.
Tarke et al. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. bioRxiv [Preprint]. 20202020.12.08.416750. https://doi.org/10.1101/2020.12.08.416750. Update in: Cell Rep Med. (2021) Jan 26; 100204. PMID: 33330869; PMCID: PMC7743077.
Cele, S. et al A. SARS-CoV-2 Omicron has extensive but incomplete escape of Pfizer BNT162b2 elicited neutralization and requires ACE2 for infection. medRxiv preprint https://doi.org/10.1101/2021.12.08.21267417.
Polack, F. P. et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 383, 2603–2615 (2020). C4591001 Clinical Trial GroupEpub 2020 Dec 10. PMID: 33301246; PMCID: PMC7745181.
Baden, L. R. et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 384, 403–416 (2021). COVE Study GroupEpub 2020 Dec 30. PMID: 33378609; PMCID: PMC7787219.
El Sahly, H. M. et al. Efficacy of the mRNA-1273 SARS-CoV-2 Vaccine at Completion of Blinded Phase. N. Engl. J. Med. 385, 1774–1785 (2021). COVE Study GroupEpub 2021 Sep 22. PMID: 34551225; PMCID: PMC8482810.
Agrati, C. et al. Coordinate Induction of Humoral and Spike Specific T-Cell Response in a Cohort of Italian Health Care Workers Receiving BNT162b2 mRNA Vaccine. Microorganisms 9, 1315 (2021). On Behalf Of The Inmi Covid-Vaccine Study GroupPMID: 34208751; PMCID: PMC8235087.
Acknowledgements
The authors gratefully acknowledge nurse staff, all the patients and all members of the HIV-VAC Study Group.
Funding
The study was performed in the framework of the SARS-CoV-2 surveillance and response program implemented by the Lazio Region Health Authority. This study was supported by funds to the Istituto Nazionale per le Malattie Infettive Lazzaro Spallanzani IRCCS, Rome (Italy), from Ministero della Salute (Programma CCM 2020; Ricerca Corrente – Linea 1 e Linea 2; COVID-2020-12371675).
Author information
Authors and Affiliations
Consortia
Contributions
A.A., A.V., and S.L. conceptualized, designed the study, and wrote the protocol. A.V. and A.C.L. wrote the first draft of the manuscript and referred to appropriate literature. A.C.L. was also the main responsible person for formal data analysis. A.A., A.C.L., A.V., C.A., C.C., F.V., and E.G. conceived, supervised the study, and contributed to data interpretation. S.C. and L.D.P. were responsible for data curation; V.P. is the main responsible of data on immunogenicity on HCWs and revised the manuscript; V.M., I.M., A.R.G., S.C. revised the manuscript content, reviewed and edited the manuscript. G.M., S.M., and F.C. performed all the serology tests and neutralization assays; V.B., E.C., and D.M. performed all the T-cell function tests; P.G., and A.M. performed and supervised the anti-SARS-CoV-2 vaccination campaign at INMI for HIV-positive individuals; R.I. and LDP enrolled participants. All authors agreed with and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Jean-Pierre Routy and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vergori, A., Cozzi Lepri, A., Cicalini, S. et al. Immunogenicity to COVID-19 mRNA vaccine third dose in people living with HIV. Nat Commun 13, 4922 (2022). https://doi.org/10.1038/s41467-022-32263-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-32263-7
This article is cited by
-
Predicting humoral responses to primary and booster SARS-CoV-2 mRNA vaccination in people living with HIV: a machine learning approach
Journal of Translational Medicine (2024)
-
The impact of the COVID-19 pandemic on people living with HIV: a cross-sectional study in Caracas, Venezuela
BMC Infectious Diseases (2024)
-
Utility of accessible SARS-CoV-2 specific immunoassays in vaccinated adults with a history of advanced HIV infection
Scientific Reports (2024)
-
Clearance of persistent SARS-CoV-2 associates with increased neutralizing antibodies in advanced HIV disease post-ART initiation
Nature Communications (2024)
-
B cell response after SARS-CoV-2 mRNA vaccination in people living with HIV
Communications Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.