Abstract
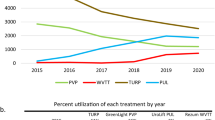
In recent years there have been more studies dedicated to Peyronie’s disease (PD). However, prevalence and incidence are likely underestimated, with limited information on regional variation in the rate of diagnosis. In this study, we sought to estimate age and regional variation of the annual incidence and prevalence of PD in the United States. We reviewed data from the IBM MarketScan™ Claims and Encounters database between 2008-2017 for men ≥18 years. Inclusion required ≥1 medical claim with PD, identified by ICD-9 and ICD-10 codes or ≥1 claim for intralesional injection for PD, identified by Current Procedure Terminology (CPT) code. Overall average annual incidence was estimated at 20.9 cases per 100,000, with the highest rate of 41.6 cases per 100,000 observed in men 55–64 years (RR = 8.2; p < 0.0001). Geographically, the highest incidence rate was observed in the South (23.9 cases per 100,000 men; RR = 1.30; p < 0.0001). Across all ages, overall prevalence of PD showed a general upward trend, from 0.052% in 2008 to 0.096% in 2017. Our findings suggest men in the southern U.S. are diagnosed more with PD compared to other regions. Identification of associated factors may allow for a more proactive approach to diagnosis and management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data archiving
SQL and R codes used to generate and analyze data are available from the corresponding author upon reasonable request.
References
Hauck EW, Weidner W. Francois de la Peyronie and the disease named after him. Lancet. 2001;357:2049–51.
Pryor JP, Ralph DJ. Clinical presentations of Peyronie’s disease. Int J Impot Res. 2002;14:414–7.
Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. Peyronie’s disease: AUA guideline. J Urol. 2015;194:745–53.
Hartzell R. Psychosexual symptoms and treatment of peyronie’s disease within a collaborative care model. Sex Med. 2014;2:168–77.
Stuntz M, Perlaky A, des Vignes F, Kyriakides T, Glass D. The prevalence of peyronie’s disease in the united states: a population-based study. PLoS ONE. 2016;11:e0150157.
Lindsay MB, Schain DM, Grambsch P, Benson RC, Beard CM, Kurland LT. The incidence of Peyronie’s disease in Rochester, Minnesota, 1950 through 1984. J Urol. 1991;146:1007–9.
Schwarzer U, Sommer F, Klotz T, Braun M, Reifenrath B, Engelmann U. The prevalence of Peyronie’s disease: results of a large survey. BJU Int. 2001;88:727–30.
DiBenedetti DB, Nguyen D, Zografos L, Ziemiecki R, Zhou X. A population-based study of Peyronie’s disease: prevalence and treatment patterns in the United States. Adv Urol. 2011;2011:282503.
Askari M, Mohamad Mirjalili SA, Bozorg M, Azizi R, Namiranian N. The prevalence of Peyronie’s disease in diabetic patients -2018- Yazd. Diabetes Metab Syndr. 2019;13:604–7.
Bjekic MD, Vlajinac HD, Sipetic SB, Marinkovic JM. Risk factors for Peyronie’s disease: a case-control study. BJU Int. 2006;97:570–4.
Butler J. Health research data for the real world: The MarketScan® databases. 2015 January 2015.
Bureau US. Do CEaSAUSC census regions and divisions of the United States. New England.
Usta MF, Bivalacqua TJ, Jabren GW, Myers L, Sanabria J, Sikka SC, et al. Relationship between the severity of penile curvature and the presence of comorbidities in men with Peyronie’s disease. J Urol. 2004;171:775–9.
Akil L, Ahmad HA. Effects of socioeconomic factors on obesity rates in four southern states and Colorado. Ethn Dis. 2011;21:58–62.
Fala L. Xiaflex (Collagenase Clostridium Histolyticum), First drug approved by the FDA for Peyronie’s disease. Am Health Drug Benefits. 2014;7:191–93.
Sun AJ, Li S, Eisenberg ML. The impact of clostridium histolyticum collagenase on the prevalence and management of Peyronie’s disease in the United States. World J Mens Health. 2019;37:234–9.
Acknowledgements
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Funding
AWP is a National Institutes of Health (NIH) K08 Scholar supported by a Mentored Career Development Award (K08DK115835-01) from the National Institute of Diabetes and Digestive and Kidney Diseases. This work is also supported in part through a Urology Care Foundation Rising Stars in Urology Award (to AWP). This study was supported by an unrestricted grant provided by Endo Pharmaceuticals Inc, Malvern, PA.
Author information
Authors and Affiliations
Contributions
OM was responsible for study design, interpretation of results and manuscript writing. JH, RD and AC were responsible for data analysis, result interpretation and manuscript revision. AWP and JMH aided in study design and planning, result interpretation, and manuscript revision. We thank the Surgical Population Analysis Research Core (SPARC), University of Utah, for its role in facilitating data collection, database management, and statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
AWP declares the following conflict(s) of interest: 1 Endo Pharmaceuticals—advisor, consultant, speaker, research support, fellowship support. 2 Antares Pharmaceuticals—advisor. 3 Bayer AG- speaker. 4 Inherent Biosciences—advisor. 5 Allotrope Medical—advisor. 6 Woven Health—founder and leadership role. 7 Vault Health—leadership role. JMH declares the following conflict(s) of interest: 1 Endo pharmaceuticals—educational and research grants. 2 Boston Scientific—educational grants. 3 StreamDx, Nanonc, Andro360—founder/own equity (early stage startups). 4 Inherent Biosciences—own equity. 5 Turtle Health—advisor. OIM, RD, JH, and AC have no conflicts of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer:
All statements in this report, including its findings and conclusions are solely those of the authors and do not necessarily represent the views of the NIH or Endo Pharmaceuticals.
Supplementary information
Rights and permissions
About this article
Cite this article
Moghalu, O.I., Das, R., Horns, J. et al. Regional variation in the incidence and prevalence of Peyronie’s disease in the United States—results from an encounters and claims database. Int J Impot Res 34, 64–70 (2022). https://doi.org/10.1038/s41443-020-00363-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-020-00363-x
This article is cited by
-
Aktuelle Behandlungskonzepte bei der Induratio penis plastica
Die Urologie (2023)