Abstract
Background/Objective:
Individuals with spinal cord injury (SCI) have been reported to have an increased prevalence of premature cardiovascular disease. Whether the increased risk of disease is owing to clustering of traditional cardiac risk factor or is over and above that predicted by risk factors was addressed.
Methods:
Ninety-one persons with chronic SCI were studied for subclinical atherosclerosis. Cardiac risk factors and coronary artery calcium (CAC) was compared to matched non-SCI controls. The 273 controls were 3:1 matched for age, gender, ethnicity and risk factors and were drawn from a national database of over 30 000 asymptomatic persons undergoing coronary scanning.
Results:
Seventy-six men and 15 women were studied. Average age was 49.7±12 years. Duration of injury was 19.7±10 years. The ethnicity of the study cohort included 36% Caucasian, 49% Latino, 10% African American, and 5% other. The mean calcium score of the SCI group was significantly greater than the control group (75±218 versus 28±104, P<0.001). The prevalence of any CAC score was greater in the SCI population than the control population (51 versus 39%, P<0.05), as was CAC score >100 (16 versus 7%, P<0.01). Women with SCI had a significantly lower CAC score than men (mean score: 12 versus 86, P<0.01).
Conclusion:
Patients with SCI were shown to have greater atherosclerotic burden than able-bodied controls. Of note, and unexplained, this finding is beyond that explained by the clustering of traditional risk factors. On the basis of these findings, increased attention should be directed toward the prevention of coronary heart disease in those with SCI.
Similar content being viewed by others
Introduction
Cardiovascular disease has been reported to be the leading cause of mortality in persons with spinal cord injury (SCI).1, 2 With improvements in acute and chronic medical management of life-threatening complications, survival of patients with SCI has improved considerably.3 As the emergence of chronic diseases increases with advancing age, health-care professionals are faced with the challenges associated with the diagnosis and management of these ailments in older individuals with SCI. With improvement in survival, it is anticipated that the prevalence of cardiovascular disease will increase, leading to greater morbidity and mortality.
Patients with SCI have been shown to have increased prevalence of coronary heart disease (CHD) risk factors such as low HDL,4, 5, 6 impaired glucose tolerance, insulin resistance and diabetes.4, 7, 8, 9 Additionally, these patients may not have symptoms despite significant CHD, partially owing to their reduced level of activity.10 Thus, it is important to identify the presence of subclinical disease in these patients to initiate appropriate treatment for the primary prevention of CHD.
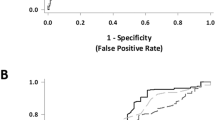
Coronary artery calcification (CAC), a component of the atherosclerotic plaque, can be accurately detected non-invasively by electron beam computed tomography (EBCT) and multi-detector computed tomography (Figure 1). There is a strong correlation between the amount of CAC and coronary plaque burden.11 CAC can be used to predict the risk of CHD in both symptomatic12 and asymptomatic subjects.13 In this study, the burden of atherosclerosis in patients with SCI was assessed by means of coronary calcification, a marker of subclinical disease.
Methods
Ninety-one persons with chronic SCI (44 with tetraplegia and 47 with paraplegia) were enrolled and compared to risk-matched non-SCI controls. The 273 controls were drawn from a database of over 30 000 asymptomatic persons undergoing coronary scanning and were matched 3:1 for age, gender, ethnicity and risk factors. Subjects with chronic SCI lay supine and underwent EBCT to acquire an image that enabled the measurement of coronary calcium. EBCT was performed with a single breath hold over 30 s. The tomographic cardiac scan consisted of at least thirty 3 mm slices. The extent of coronary calcium (volume score), mean calcium scores, and prevalence of coronary calcium calcification was assessed.
Blood was collected and sent to the medical center chemistry laboratory for serum lipid determination. A health questionnaire to determine the presence or absence of angina, exercise and depression was administered.
Statistical analysis
Distributions of demographics, cardiovascular risk factors and the various calcium scores were compared across patients with SCI and controls. Differences in characteristics were compared using ANOVA for continuous variables and χ2 tests for categorical variables. The following covariates were used in a backward stepwise regression for multivariable adjustment: age, gender, body mass index, (BMI) high cholesterol, lipid lowering medication, smoking, hypertension, diabetes mellitus and spinal injury level (cervical or thoracic). A severe CAC score was defined as >400. Among those with detectable CAC, the relationship between risk factors and the quantity of calcification ((ln)Agatston score) was assessed with multivariable linear regression, controlled for all other risk factors in the model. Statistical analyses were performed with SPSS 13.0.1 software for Windows (SPSS Inc, Chicago, IL, USA) and STATA 8.0 for Windows (Stata Co, College Station, TX, USA).
Results
Seventy-six males and 15 females with SCI were studied. The mean age of the study population was 49.7±12 years (range 20–90 years). The study population consisted of 49% Hispanics, 36% Caucasians, 10% African-Americans, and 5% other. Duration of injury was 19.7±10 years (range XX–XX years). Hypertension was present in 12% and diabetes mellitus, in 7%. The mean LDL cholesterol and HDL cholesterol concentrations were 119 mg/dl, and was 42 mg/dl respectively. A positive family history for coronary artery disease (CAD) was reported in 35% of the subjects. Past or current cigarette smoking was present in 10%. Statins were being used in 7% of the population.
The mean calcium score of the SCI group was significantly greater than the control group (75±218 versus 28±104, P<0.001). The prevalence of any CAC was greater in the SCI group than the control group (51 versus 39%, P<0.05), as was a CAC score >100 (16 versus 7%, P<0.01). Women with SCI had significantly less CAC than men (mean score 12 versus 86, P<0.01).
Persons with tetraplegia had a greater prevalence of severe CAC scores than those with paraplegia (6.8 versus 2.1%, P<0.05). After controlling for all risk factors, those with tetraplegia also had a trend for higher CAC scores (eg, score >100) compared with those with paraplegia (13.6 versus 6.4%, P=0.06).
Discussion
This is the first study reporting the quantification of coronary calcification by EBCT in individuals with SCI. Persons with SCI had increased coronary calcification compared to able-bodied controls who were matched for age, gender, ethnicity and risk factors, indicating that they have greater atherosclerosis than that predicted by the clustering of traditional risk factors.
CHD is now a major cause of morbidity and mortality in patients with SCI.1, 2 A recent survey has reported that CHD has become the leading cause of death in veterans with chronic SCI (unpublished information, SCI QUERI). A higher prevalence of CHD has been reported in individuals with duration of SCI greater than 10 years compared with relatively healthy age-matched controls.14 The reduction in level of activity and adverse changes in body composition reported in those with chronic SCI have profound metabolic consequences which may influence the prognosis and severity of CAD. Metabolic sequela of SCI include disorders of carbohydrate and lipid metabolism. Depressed values of HDL have been reported in patients with SCI compared with able-bodied subjects,4, 5, 6, 15 which may be owing to increased proportion of adipose tissue,16, 17 extremely low levels of physical activity,15, 18, 19 and time since injury.15, 20, 21 Bauman22 has shown that those with tetraplegia have lower serum HDL levels than those with paraplegia. Studies have reported triglyceride levels to be 6–60% higher in patients with SCI, although this did not reach statistical significance in all studies, nor was it found in others.4, 5, 6, 7, 23, 24, 25 In persons with SCI, as has been reported in the general literature, a direct relationship has been demonstrated between abdominal circumference (AC) and serum triglyceride concentration, as well as an inverse relationship between AC and serum HDL cholesterol levels.26 Patients with SCI have also been shown to have increased prevalence of impaired glucose tolerance, insulin resistance and diabetes, owing to the aforementioned adverse changes in body composition and, potentially, unknown causes.4, 7, 8, 9 Other previously reported CHD risk factors after SCI include decreased physical activity, psychosocial factors of depression and social isolation,27 elevated plasma homocysteine,28 and increased levels of C-reactive protein.29, 30 In addition, evidence suggests that persons with chronic SCI have a circulating heavy-chain IgG that is the cause of loss of high-affinity prostacyclin receptors in platelets, which results in the absence of prostaglandin-induced inhibition of platelet-stimulated thrombin generation; furthermore, this IgG fragment is heterophilic, binding the platelet insulin receptor and blocking platelet nitric oxide synthesis.31, 32
It is conceivable that autonomic dysreflexia (AD) in some individuals may play a role in increasing the risk of CVD owing to repeated episodes of vascular contraction and associated hypertension, occasionally of extreme levels.33 AD occurs almost exclusively in those with SCI rostral to the T6 level. However, Groah et al.34 reported an inverse relationship between level of SCI and CHD, which does not preclude the influence of AD on vascular disease progression in those with tetraplegia but highlights the importance of other risk factors in those with paraplegia that may overshadow its presence.
Patients with SCI may not have symptoms of angina pectoris despite significant CAD, partially owing to their reduced level of activity. Additionally, individuals with SCI rostral to T4 may not recognize cardiac pain owing to disruption of sympathetic afferent fibers branching with cardiac pain fibers. SCI patients often undergo rehabilitation programs, exercise training, metabolic testing, and surgical procedures without having their cardiac status assessed, which may pose a significant potential, unpredictable risk. Thus the diagnosis of CHD in patients with SCI requires heightened clinical suspicion.
Bauman et al.35 assessed the presence of latent CHD in 20 asymptomatic subjects with paraplegia by non-invasive arm ergometry exercise stress testing and radionuclide tomographic imaging; 62% of paraplegics without known CHD had scintigraphic evidence of ischemia as compared with 26% diagnosed with ischemia by exercise stress testing alone. In another study, in a relatively young sample of men with tetraplegia who had several risk factors for CHD, Bauman et al.36 used radionuclide myocardial imaging with thalium-201 to assess myocardial ischemia and found that approximately half the subjects had latent CHD without previous symptoms or abnormal EKGs. In a similar fashion, Lee et al10 found that 63.8% of clinically asymptomatic patients with paraplegia or quadriplegia had evidence of ischemia on myocardial perfusion imaging after dipyridamole administration. In addition, SCI patients with a higher level (quadriplegia) and severity of SCI (complete) had increased risk of ischemia.10 Therefore, the actual risk of CHD may be greater than previously assumed in those with SCI, with subclinical disease accounting for a significant proportion of CHD.
The results of this study should be interpreted in the light of some limitations. This is a cross-sectional study in which subclinical atherosclerosis was measured by coronary calcification, with the absence of clinical events being a weakness of this investigation. However, it should be recognized that CAC has been shown to predict coronary events in both symptomatic12 as well as asymptomatic13 populations. In our study, CHD risk factors were self-reported. Hoff et al37 suggested that self reported CHD risk factors are reliable. A new scientific statement from the American Heart Association reiterates that CAC can be used as a screening test for cardiovascular risk, and this determination adds incremental predictive value to traditional risk factors.38 However, potential residual confounding factors cannot be excluded. A possible confounder, not evaluated in this study, is BMI kg/m2. It has been suggested that higher BMI could increase noise in EBCT scans and increase CAC values spuriously.39 In our study, persons with an average duration of injury of 19.7 years, which may have increased relative adiposity, but in those with chronic SCI, BMI is generally not increased 24.40 Because survival bias would have eliminated those individuals with CHD mortality before entry into the study, the risk of cardiac disease may have been underestimated.
In this study, persons with SCI had more atherosclerotic burden than ambulatory, able-bodied controls, over and above that predicted by the clustering of traditional risk factors. Coronary calcium appears to be more prevalent and occurs with greater severity in the subjects with chronic SCI compared with age-, ethnicity- and risk factor-matched controls. Prospective studies are needed to evaluate whether the increased CAC in patients with SCI is associated with increased CHD events. However, based on these findings, more attention and therapy in those with SCI should be directed at prevention of CHD. Therefore, an aggressive cardiac prevention program should be instituted in patients with SCI as part of their rehabilitation. Modifiable risk factors, such as obesity, inactivity, dietary factors, and smoking, should be addressed to lower the risk of CAD in this high risk population.
References
DeVivo MJ, Stover SL . Long-term survival and causes of death. In: Stover SL, DeLisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen: Gaithersbug, MD 1995, pp 289–316.
Hartkoop A, Bronnum-Hansen H, Seidenschnur AM, Biering-Sorensen F . Survival and cause of death after traumatic spinal cord injury. A long-term epidemiological survey from Denmark. Spinal Cord 1997; 35: 76–85.
DeVivo MJ, Black KJ, Stover SL . Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993; 74: 248–254.
Demirel S, Demirel G, Tukek T, Erk O, Yilmaz H . Risk factors for coronary heart disease in patients with spinal cord injury in Turkey. Spinal Cord 2001; 39: 134–138.
Bauman WA et al. Coronary artery disease: metabolic risk factors and latent disease in individuals with paraplegia. Mt Sinai J Med 1992; 59: 163–168.
Schmid A et al. Lipoproteins and free plasma catecholamines in spinal cord injured men with different injury levels. Clin Physiol 2000; 20: 304–310.
Karlsson AK . Insulin resistance and sympathetic function in high spinal cord injury. Spinal Cord 1999; 37: 494–500.
Bauman WA, Adkins RH, Spungen AM, Waters RL . The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord 1999; 37: 765–771.
Tharion G, Prasad KR, Gopalan L, Bhattachargi S . Glucose intolerance and dyslipidaemias in persons with paraplegia and tetraplegia in south India. Spinal Cord 1998; 36: 228–230.
Lee CS, Lu YS, Lee ST, Lin CC, Ding HJ . Evaluating the prevalence of silent coronary artery disease in asymptomatic patients with spinal cord injury. Int Heart J 2006; 47: 325–330.
Rumberger JA et al. Coronary artery calcium area by electron beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation 1995; 92: 2157–2162.
Budoff MJ . Prognostic value of coronary artery calcification. Vasc Dis Prev 2005; 2: 2–10.
Raggi P et al. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation 2000; 101: 850–855.
Yekutiel M, Brooks ME, Ohry A, Yarom J, Carel R . The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia 1989; 27: 58–62.
Brenes G, Dearwater S, Shapera R, LaPorte RE, Collins E . High density lipoprotein cholesterol concentrations in physically active and sedentary spinal cord injured patients. Arch Phys Med Rehabil 1986; 67: 445–450.
Maki KC et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia 1995; 33: 102–109.
Kocina P . Body composition of spinal cord injured adults. Sports Med 1997; 23: 48–60. Review.
Dearwater SR, LaPorte RE, Robertson RJ, Brenes G, Adams LL, Becker D . Activity in the spinal cord-injured patient: an epidemiologic analysis of metabolic parameters. Med Sci Sports Exerc 1986; 18: 541–544.
Dallmeijer AJ, Hopman MT, van der Woude LH . Lipid, lipoprotein, and apolipoprotein profiles in active and sedentary men with tetraplegia. Arch Phys Med Rehabil 1997; 78: 1173–1176.
Walker J, Shepherd RJ . Cardiac risk factors immediately following spinal injury. Arch Phys Med Rehabil 1993; 74: 1129–1133.
Dallmeijer AJ, van der Woude LH, van Kamp GJ, Holander AP . Changes in lipid, lipoprotein and apolipoprotein profiles in persons with spinal cord injuries during the first 2 years post-injury. Spinal Cord 1999; 37: 96–102.
Bauman WA, Adkins RH, Spungen AM, Kemp BJ, Waters RL . The effect of residual neurological deficit on serum lipoproteins in individuals with chronic spinal cord injury. Spinal Cord 1998; 36: 13–17.
Bauman WA, Spungen AM . Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: A model of premature aging. Metabolism 1994; 43: 749–756.
Bauman WA et al. The effect of residual neurological deficit on serum lipoprotein profiles in persons with chronic spinal cord injury. Spinal Cord 1998; 36: 13–17.
Bauman WA et al. Is immobilization associated with an abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord 1999; 37: 485–493.
Maki KC et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia 1995; 33: 102–109.
Bombarier CH et al. Symptoms of major depression in people with spinal cord injuries: implications for screening. Arch Phys Med Rehabil 2004; 85: 1749–1756.
Bauman WA, Adkins RH, Spungen AM . Levels of plasma homocysteine in a population of persons with spinal cord injury. J Spinal Cord Med 2001; 24: 81–86.
Lee MY et al. C-reactive protein, metabolic syndrome, and insulin resistance in individuals with spinal cord injury. J Spinal Cord Med 2005; 28: 20–25.
Sabharwal S . Cardiovascular dysfunction in spinal cord disorders. In Lin VW (ed). Spinal Cord Medicine. Demos Medical Publishing, Inc., New York 2003, pp 179–192.
Kahn NN, Bauman WA, Sinha AK . Loss of high-affinity prostacyclin receptors in platelets and the lack of prostaglandin-induced inhibition of platelet-stimulated thrombin generation in subjects with spinal cord injury. Proc Natl Acad Sci USA 1996; 93: 245–249.
Kahn NN, Bauman WA, Sinha AK . Circulating heavy-chain IgG, a pathological mediator for coronary artery disease, recognizes platelet surface receptors of both prostacyclin and insulin. Platelets 2003; 14: 203–210.
Spungen AM, Wang J, Pierson Jr RN, Bauman WA . Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol 2000; 88: 1310–1315.
Groah SL, Weitzenkamp D, Sett P, Soni B, Savic G . The relationship between neurological level of injury and symptomatic cardiovascular disease risk in the aging spinal injured. Spinal Cord 2001; 39: 310–317.
Bauman WA, Raza M, Spungen AM, Machac J . Cardiac stress testing with thallium-201 imaging reveals silent ischemia in individuals with paraplegia. Arch Phys Med Rehabil 1994; 75: 946–950.
Bauman WA, Raza M, Chayes Z, Machac J . Tomographic thallium-201 myocardial perfusion imaging after intravenous dipyridamole in asymptomatic subjects with quadriplegia. Arch Phys Med Rehabil 1993; 74: 740–744.
Hoff JA, Daviglus ML, Chomka EV, Krainik AJ, Sevrukov A, Kondos GT . Conventional coronary artery disease risk factors and coronary artery calcium detected by electron beam tomography in 30,908 healthy individuals. Ann Epidemiol 2003; 13: 163–169.
Budoff MJ et al. Assessment of Coronary Artery Disease by Cardiac Computed Tomography, a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 2006; 114: 1761–1791.
Sevrukov A, Pratap A, Doss C, Jelnin V, Hoff A, Kondos GT . Electron beam tomography imaging of coronary calcium: the effect of body mass index on radiologic noise. J Comput Assist Tomogr 2002; 26: 592–597.
Spungen AM et al. Factors influencing body composition in persons with spinal cord injury: A cross-sectional study. J Amer Physiol 2003; 95: 2398–2407.
Author information
Authors and Affiliations
Additional information
Sponsored: Paralyzed Veterans of America's Spinal Cord Research Foundation – Grant Number 1960-03
Rights and permissions
About this article
Cite this article
Orakzai, S., Orakzai, R., Ahmadi, N. et al. Measurement of coronary artery calcification by electron beam computerized tomography in persons with chronic spinal cord injury: evidence for increased atherosclerotic burden. Spinal Cord 45, 775–779 (2007). https://doi.org/10.1038/sj.sc.3102045
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102045
Keywords
This article is cited by
-
The neurological level of spinal cord injury and cardiovascular risk factors: a systematic review and meta-analysis
Spinal Cord (2021)
-
Increased risk of sensorineural hearing loss in patients with spinal cord injury: a nationwide longitudinal follow-up study
Spinal Cord (2021)
-
An arterial insufficiency ulcer in an individual with cervical spinal cord injury and hypotension
Spinal Cord Series and Cases (2020)
-
Guideline for the identification and management of cardiometabolic risk after spinal cord injury: a case of unsubstantiated recommendations
Spinal Cord Series and Cases (2019)
-
Coronary artery disease and hypertension in a non-selected spinal cord injury patient population
Spinal Cord (2017)