Abstract
Introduction:
It is not known whether very preterm infants born to preeclamptic women have worse outcomes than those delivered preterm for other causes.
Objective:
We assessed the association between preeclampsia (PE) and the neonatal morbidity and mortality of very preterm infants.
Methods:
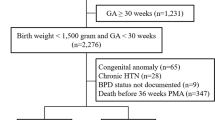
Over 2015 and 2016, 11 collaborating Portuguese level III NICUs prospectively enrolled a cohort of mothers with or without PE who delivered liveborn premature infants between 24 and 30 completed weeks of gestation. Data on neonatal morbidities were collected and their association to PE was assessed.
Results:
The final cohort consisted of 410 mothers who delivered 494 preterm infants. Infants from PE mothers weighed less than those of non-PE mothers (819 ± 207 g vs. 989 ± 256 g, p < 0.0001). Incidences of respiratory distress syndrome, patent ductus arteriosus, early and nosocomial sepsis, necrotizing enterocolitis, pneumonia, meningitis, retinopathy of prematurity, intraventricular hemorrhage, periventricular infarction, periventricular leukomalacia, and mortality did not differ significantly between infants of PE or non-PE mothers. Incidence of bronchopulmonary dysplasia (BPD—defined as oxygen dependency at 36 weeks) was higher in PE infants compared with non-PE infants by both univariate and multivariate logistic regression (p = 0.007).
Conclusion:
We conclude that, when controlling for gestational age, maternal PE results in higher incidence of only BPD among preterm Portuguese infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
03 August 2018
Text for Correction
References
Sibai B, Dekker G, Kupfermine M. Pre-eclampsia. Lancet. 2005;365:785–99.
Dulley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33:130–7.
Silasi M, Cohen B, Karumanchi AS, Rana S. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin North Am. 2010;37:239–53.
Rugolo L, Bentlin M, Trindade C. Preeclampsia: effect on the fetus and newborn. NeoReviews 2011;12 Issue 4.
Szymonowicz W, Yu VY. Severe pre-eclampsia and infants of very low birth weight. Arch Dis Child. 1987;62:712–6.
Tokumasu H, Tokumasu S, Kawakami K. Impact of pre-eclampsia in extremely premature infants: population-based study. Pediatr Int. 2016;58:578–83. https://doi.org/10.1111/ped.12905
Cetinkaya M, Ozkan H, Koksal N. Maternal preeclampsia is associated with increased risk of necrotizing enterocolitis in preterm infants. Early Hum Dev. 2012;88:893–8. https://doi.org/10.1016/j.earlhumdev.2012.07.004
Ozkan H, Cetinkaya M, Koksal N, Ozmen A, Yıldız M. Maternal preeclampsia is associated with an increased risk of retinopathy of prematurity. J Perinat Med. 2011;39:523–7. https://doi.org/10.1515/JPM.2011.071
Ozkan H, Cetinkaya M, Koksal N. Increased incidence of bronchopulmonary dysplasia in preterm infants exposed to preeclampsia. J Matern Fetal Neonatal Med. 2012;25:2681–5. https://doi.org/10.3109/14767058.2012.708371
Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. J Pregnancy. 2011;214365. https://doi.org/10.1155/2011/214365.
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–31. https://doi.org/10.1097/01.AOG.0000437382.03963.88
National Institutes of Health (NIH). Consensus Development Panel on the effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA. 1995;273:413–8.
Magee L, Sawchuck D, Synnes A, von Dadelszen P. SOGC Clinical Practice Guideline. Magnesium sulphate for fetal neuroprotection. J Obstet Gynaecol Can. 2011;33:516–29.
Hagberg H, Wennerholm UB, Sävman K. Sequelae of chorioamnionitis. Curr Opin Infect Dis. 2002;15:301–6.
Blanc WA. Pathology of the placenta, membranes and umbilical cord in bacterial, fungal and viral infections in man. In: Naeye RL, Kissane JM, editors. International Academy of Pathology Monograph. Perinatal Diseases by 14 authors. Baltimore: William and Wilkins; 1981.
Matijevic R, Olujic B, Tumbri J, Kurjak A. Cervical incompetence: the use of selective and emergency cerclage. J Perinat Med. 2001;29:31–5.
Tikkanen M. Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand. 2011;90:140–9. https://doi.org/10.1111/j.1600-0412.2010.01030
MacDonald H. American Academy of Pediatrics. Committee on Fetus and Newborn. Perinatal Care at the Threshold of Viability. Pediatrics. 2002;110:1024–7.
Ballard JL, Khoury JC, Wedig K, Wang L, Eilers-Walsman BL, Lipp R. New Ballard Score, expanded to include extremely premature infants. J Pediatr. 1991;119:417–23.
Fenton TR. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome - 2016 Update. Neonatology. 2017;111:107–25. https://doi.org/10.1159/000448985
Saugstad OD, Aune D. Optimal oxygenation of extremely low birth weight infants: a meta-analysis and systematic review of the oxygen saturation target studies. Neonatology. 2014;105:55–63. https://doi.org/10.1159/000356561
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Salazar A, Guedes A, Álvares S, Baptista MJ, Soares P, Morais S, et al. National consensus on the diagnostic and therapeutic approach to ductus arteriosus in the preterm newborn. Portuguese Society of Neonatology, 2010. www.lusoneonatologia.com
Program of epidemiological surveillance of nosocomial infection in neonatal intensive care units in Portugal, 2007. https://www.dgs.pt/programa...de...infeccao/.../ucin-protocolo-pdf.aspx
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179–201.
An International Classification Of Retinopathy Of Prematurity. Pediatrics 1984;74:127–33.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Volpe JJ. Neurology of the newborn. 4th ed. Philadelphia: WB Saunders; 2001. p. 428–93.
de Vries L, Rennie JM. Preterm brain injury. In: Rennie JM, Roberton NRC, editors. Textbok of neonatology. 3rd ed. London: Churchill Livingstone; 1999. p. 1252–70.
Borzychowski AM, Saegent IL, Redman CWG. Inflammation and pre-eclampsia. Semin Fetal Neonatal Med. 2006;11:309–16.
Dikensory E, .Balat O, Pence S, Balat A, Cekmen M, Yurekli M. The changes of plasma malondialdehyde, nitric oxide, and adrenomedullin levels in patients with preeclampsia. Hypertens Pregnancy. 2009;28:383–9.
Howlader ZH, Parveen S, Tamanna S, Khan TA, Begum F. Oxidative stress and antioxidante status in neonates born to preeclamptic mother. J Trop Pediatr. 2009;55:363–7.
Romero R, Nien JK, Espinoza J, Todem D, Fu W, Chung H, et al. A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J Matern Fetal Neonatal Med. 2008;21:9–23. https://doi.org/10.1080/14767050701830480
Goyal R, Yellon SM, Longo LD, Mata-Greenwood E. Placental gene expression in a rat ‘model’ of placental insufficiency. Placenta. 2010;31:568–75. https://doi.org/10.1016/j.placenta.2010.05.004
Trindade CP, Rugolo LS. Free radicals and neonatal diseases. Neoreviews. 2007;8:522–32.
Hansen AR, Barnes CM, Folkman J, McElrath TF. Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr. 2010;156:532–6. https://doi.org/10.1016/j.jpeds.2009.10.018
O’Shea JE, Davis PG, Doyle LW, Victorian Infant Collaborative Study Group. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr Res. 2012;71:210–4. https://doi.org/10.1038/pr.2011.27
Soliman N, Chaput K, Alshaikh B, Yusuf K. Preeclampsia and the risk of Bronchopulmonary Dysplasia in preterm infants less than 32 weeks gestation. Am J Perinatol. 2017;34:585–92. https://doi.org/10.1055/s-0036-1594017
Li Y, Cui Y, Wang C, Liu X, Han J. A risk factor analysis on disease severity in 47 premature infants with bronchopulmonary dysplasia. Intractable Rare Dis Res. 2015;4:82–6. https://doi.org/10.5582/irdr.2015.01000
Bland RD. Neonatal chronic lung disease in the post-surfactant era. Biol Neonate. 2005;88:181–91.
Kramer BW, Kallapur S, Newnham J, Jobe AH. Prenatal inflammation and lung development. Semin Fetal Neonatal Med. 2009;14:2–7.
Jobe AH, Kallapur SG. Chorioamnionitis, surfactant, and lung disease in very low birth weight infants. J Pediatr. 2010;156:3–4.
Guimarães H, Rocha G, Vasconcellos G, Proença E, Carreira ML, Sossai MR, et al. Risk factors for bronchopulmonary dysplasia in five Portuguese neonatal intensive care units. Rev Port Pneumol. 2010;16:419–30.
Cunha GS, Mezzacappa-Filho F, Ribeiro JD. Risk factors for bronchopulmonary dysplasia in very low birth weight newborns treated with mechanical ventilation in the first week of life. J Trop Pediatr. 2005;51:334–40.
Bose C, Van Marter LJ, Laughon M, O’Shea TM, Allred EN, Karna P, et al. Extremely Low Gestational Age Newborn Study Investigators. Fetal growth restriction and chronic lung disease among infants born before the 28th week of gestation. Pediatrics. 2009;124:e450–8. https://doi.org/10.1542/peds.2008-3249
Abman SH. Bronchopulmonary dysplasia: a vascular hypothesis. Am J Respir Crit Care Med. 2001;164:1755–6.
Thébaud B, Lacaze-Masmonteil T. If your placenta doesn’t have it, chances are your lungs don’t have it either: the “vascular hypothesis” of bronchopulmonary dysplasia starts in utero. J Pediatr. 2010;156:521–3. https://doi.org/10.1016/j.jpeds.2009.12.015
Author Contributions
Collaborators of the Hypertensive Disorders of Pregnancy Study Group: Elisa Proença, Carmen Carvalho, Luís Guedes Martins (Centro Materno Infantil do Norte, Porto, Portugal); Teresa Martins (Hospital Pedro Hispâno, Matosinhos, Portugal); Alice Freitas, Clara Paz Dias (Hospital da Senhora da Oliveira, Guimarães, Portugal); Albina Silva, Almerinda Barroso (Hospital de Braga, Braga, Portugal); Isabel Diogo, Gonçalo Cassiano, Helena Ramos (Centro Hospitalar Lisboa Central, Maternidade Dr Alfredo da Costa, Lisboa, Portugal); Maria Margarida Abrantes, Paula Costa (Centro Hospitalar Lisboa Norte, Hospital de Santa Maria, Lisboa, Portugal); Anabela Salazar, Filipa Vieira, Dora Fontes (Centro Hospitalar Lisboa Ocidental, Hospital São Francisco Xavier, Lisboa, Portugal); Rosalina Barrosos, Tânia Marques (Hospital Prof. Dr Fernando Fonseca, Amadora, Portugal, Portugal); Vera Santos, Ecaterina Scortenschi, Celeste Santos, Fernanda Vilela (Centro Hospitalar do Algarve, Hospital de Faro, Faro, Portugal); Conceição Quintas (Centro Hospitalar de Vila Nova de Gaia/ Espinho, Hospital de Vila Nova de Gaia, Vila Nova de Gaia, Portugal)
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
A full list of authors appear in the Author Contributions
Rights and permissions
About this article
Cite this article
Rocha, G., de Lima, F.F., Machado, A.P. et al. Preeclampsia predicts higher incidence of bronchopulmonary dysplasia. J Perinatol 38, 1165–1173 (2018). https://doi.org/10.1038/s41372-018-0133-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0133-8
This article is cited by
-
Early Fetal Growth Restriction with or Without Hypertensive Disorders: a Clinical Overview
Reproductive Sciences (2024)
-
Perinatal origins of bronchopulmonary dysplasia—deciphering normal and impaired lung development cell by cell
Molecular and Cellular Pediatrics (2023)
-
Maternal hypertensive disorders and survival without major morbidities among extremely low gestation newborns
Journal of Perinatology (2023)
-
Respiratory responses to hypoxia during rest and exercise in individuals born pre-term: a state-of-the-art review
European Journal of Applied Physiology (2022)